It turns out that a fair number of people get CV-19 in the hospital. As Dave mentions, this post was sparked by a Star Tribune story today. Please note carefully that this database only counts people who have been in the hospital for 14 days or more. That is very misleading. Anyone who has a positive test upon or after admission should be included, and only taken out if their primary treatment turns out to be for CV-19. That method would allow inclusion of incidental hosps and nocosomial, or hospital-acquired, infections. Very few people are in the hospital for 14 days. If you test positive the first time after 3 days in the hospital, you got it in the hospital. So the 4% or 10% of hospitalizations is a very substantial undercount. I would guess that at least 20% of hospitalizations attributed to CV-19 involve infections acquired in the hospital, and another even larger percent are incidental. The hospitals and state governments have the data; they should all release it. There is an effort underway by the current federal administration to accomplish this, we are told. Why–all part of the desperate backtracking to improve poll numbers before the mid-terms. I think what this may actually accomplish is to make it clear to people that they were unduly and intentionally terrified for two years about hospitalization risks.
Dave’s notes:
- In the Minneapolis Star Tribune on 2/8/2022 Jeremy Olson reported that in January, 2022 “more than 60 COVID-19 cases per day in mid-January of patients whose infections presumably occurred after admission, according to federal data”. The article is available here: https://www.startribune.com/
severe-covid-19-at-lowest- levels-in-months-in-minnesota- hospitals/600144482/ . Although Jeremy does not state the source of this data, this reference to Covid infections which occur after admissions reminded us that we had seen this data in a database before, and prompted us to find it. - The US Department of Health and Human Services publishes a database titled “COVID-19 Reported Patient Impact and Hospital Capacity by State Timeseries” here: https://healthdata.gov/
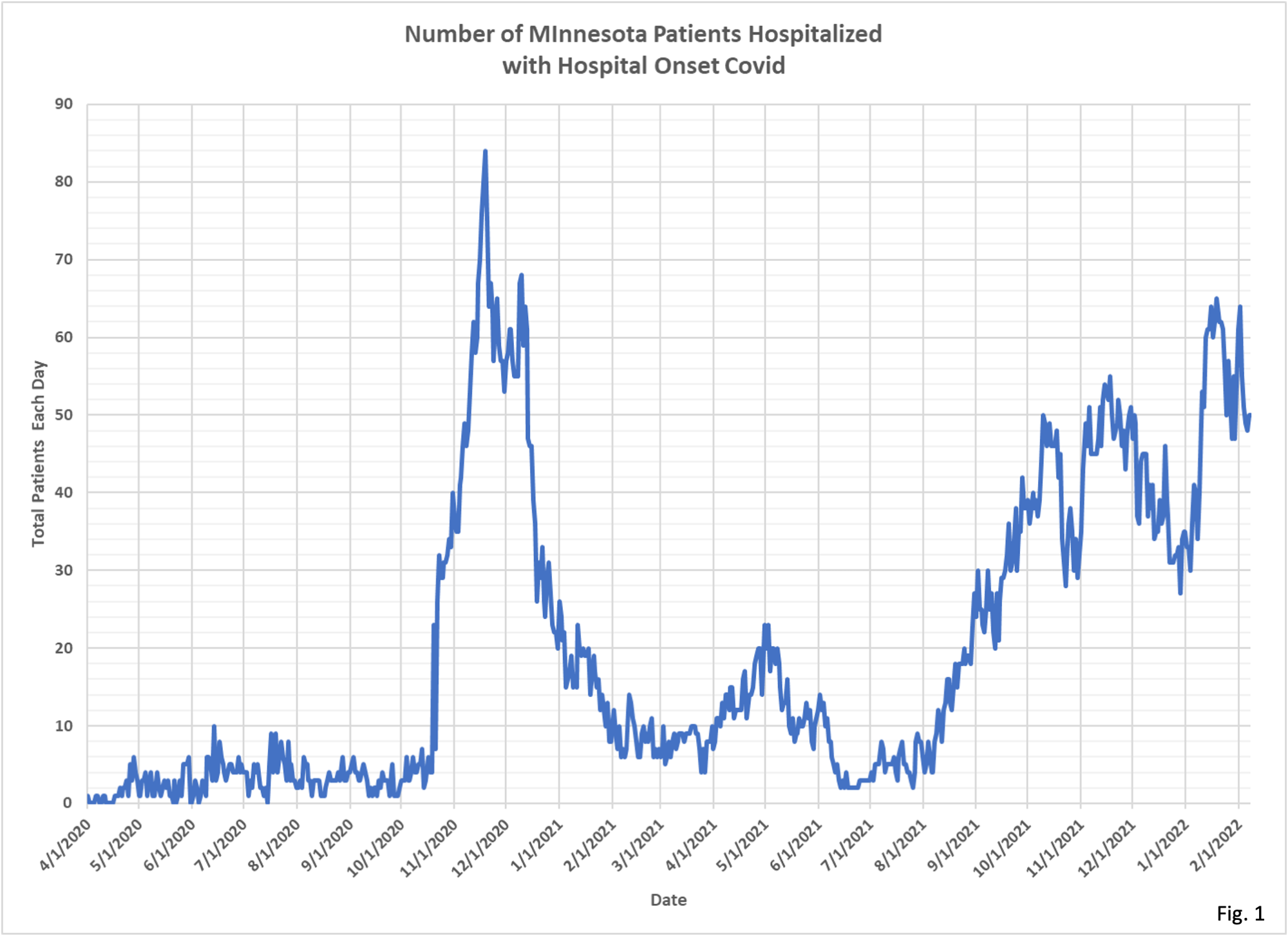
Hospital/COVID-19-Reported- Patient-Impact-and-Hospital- Capa/g62h-syeh This database, in Column 9, contains a number series named “hospital_onset_covid”, defined as “Total current inpatients with onset of suspected or laboratory-confirmed COVID-19 fourteen or more days after admission for a condition other than COVID-19 in this state.” This data set for hospital onset covid, when filtered for Minnesota, is plotted in Fig. 1. We can see that in mid-January 2022 the number of hospital onset covid patients in Minnesota is indeed between 60 and 65, leading us to believe that this is the database that Jeremy Olson used for the reference in his article. - Note that the number of Hospital Onset Covid patients is the total number of patients who have been hospitalized for 14 days, then test positive for Covid, and are still hospitalized on any given day. This is not the number of patients per day who test positive for Covid after having been hospitalized for 14 days, which is how Jeremy’s wording reads to us.
- Note also that Hospital Onset Covid patients are completely different from incidental Covid cases, where a patient is admitted for a non-Covid condition and then immediately tests positive for Covid. It is believed that incidental Covid cases are a substantial fraction of daily Covid admissions, based on data published in other states. We have submitted a Data Practice Act request for incidental Covid data, but so far have not received anything from the Minnesota Department of Health (MDH).
- In Fig. 1 we can see that on 1/19/2022 there were 65 patients who had been in the hospital for 14 or more days before testing positive. Hospital Onset Covid patients were highest during the time of the late 2020 surge in Covid cases. In 2021 the number of Hospital Onset Covid patients appears largely proportional to cases during the Delta variant surge until early December 2021. There is a modest rise in Hospital Onset Covid patients in January 2022, but so far the rise is nowhere near to proportional to the surge in Omicron variant Covid cases.
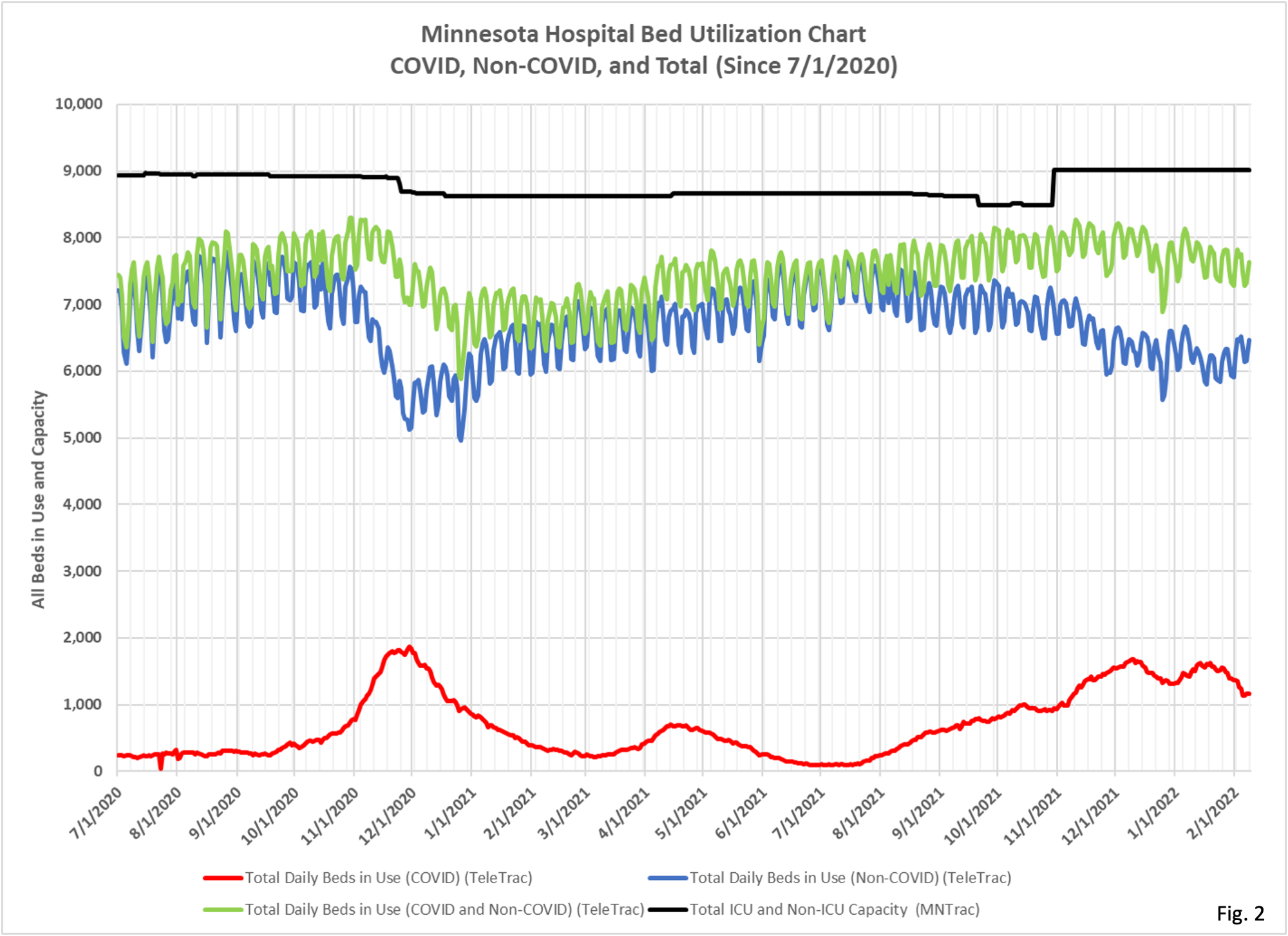
- In Fig. 2 we display the number of Covid patients hospitalized in Minnesota on each day (red curve). In January 2022 there were an average of 1499 Covid patients hospitalized in Minnesota each day. If 65 of these patients were infected 14 or more days after being admitted, this would represent 4.3% of all hospitalized Covid patients.
- In Fig. 2 we also display the total number of patients hospitalized in Minnesota for non-Covid reasons (blue curve). These are the number of patients, if they were to be hospitalized for 14 days, who would be the pool of people who might possibly be subject to Hospital Onset Covid. This data is taken from the TeleTrac data file available on the Minnesota Response Capacity web page here: https://mn.gov/covid19/data/
response-prep/response- capacity.jsp . From the underlying data for Fig. 2 the average number of non-Covid hospital beds in use in January 2022 was 6,180 beds per day. If 10% of these patients were hospitalized for 14 or more days that would equal 618 potential Hospital Onset Covid patients. With this set of assumptions 65 out of 618 patients would test positive for Covid 14 or more days after admission, or 10.5% of patients. While we don’t know how many non-Covid patients are hospitalized 14 or more days hopefully our guess of 10% of total patients is a good starting point until we obtain further information.


this entire epidemic the hospitals have been the primary super spreaders “events” of the virus …
This would give hospitals cover for their “don’t come in until your lips turn blue” policies.
On the other hand, if therapeutics weren’t poo-pooed by Fauci et al, even fewer people would have gone to hospital emergency rooms in the first place.
LA County keeps a public database of outbreaks in schools and at businesses. You can look up if your local Costco had an outbreak. But, they do not list outbreaks in hospitals. Early on, it was angering nurses and doctors, who were bearing the brunt of the pandemic without a clue about what their risks were for getting C19 at work.
No doubt folks are getting infections of various kinds in hospitals, but with the covid testing madness, how many of these are false or low positives? As noted here often, case counts are always dubious and the only cases that really matter are those that cause serious health problems. A further confounder is multiple tests. How are those results handled when there is financial incentive to count as many covid cases as possible? E.g., a neighbor spent a few weeks in the hospital (surgery) about 2 years ago and had 3 covid tests over his first 4 days in the hospital – negative, positive, negative.
the testing has been, is and will be a problem, there is no doubt of that. Your neighbor’s experience is not unusual, was he ever really “infected”, probably not, but he will be treated as a case.
While some (many?) patients who test negative on admission but positive on subsequent tests while inpatients may be false-positive or may have been incubating the virus on the day of admission (tho this would not apply to the study above that only counted folks after day14) there is another reason why hospital based transmission is widespread: My 1100 bed center transports clinically infected C19 patients around the hospital with only surgical masks, often poorly fitted! (Not that the masks would do anything anyway). Rational? The MBAs decided that since they could not “fit test” every C19 patient, there was no point in even giving them N95s. So we 5 year olds in school, restaurant servers at high-end galas but not the wealthy attendees, and leftie politicians are mask-exempt but C19(+) patients with temps of 102, vicious cough, and a low cycle threshold are transported around the hallways like they are healthy JCAHO inspectors. This is the result of MBAs taking over hospital leadership instead of physicians, this is corporate medicine (whether for-profit or “not-for -profit for profit” [ie the profit of administrators who make these stupid decisions]).
Secondly, the study above having counted only patients after day 14 of hospitalization (as Keven alludes) vastly underestimates the actual nosocomial acquisition rate.
thank you for reading, and for the very knowledgeable comments