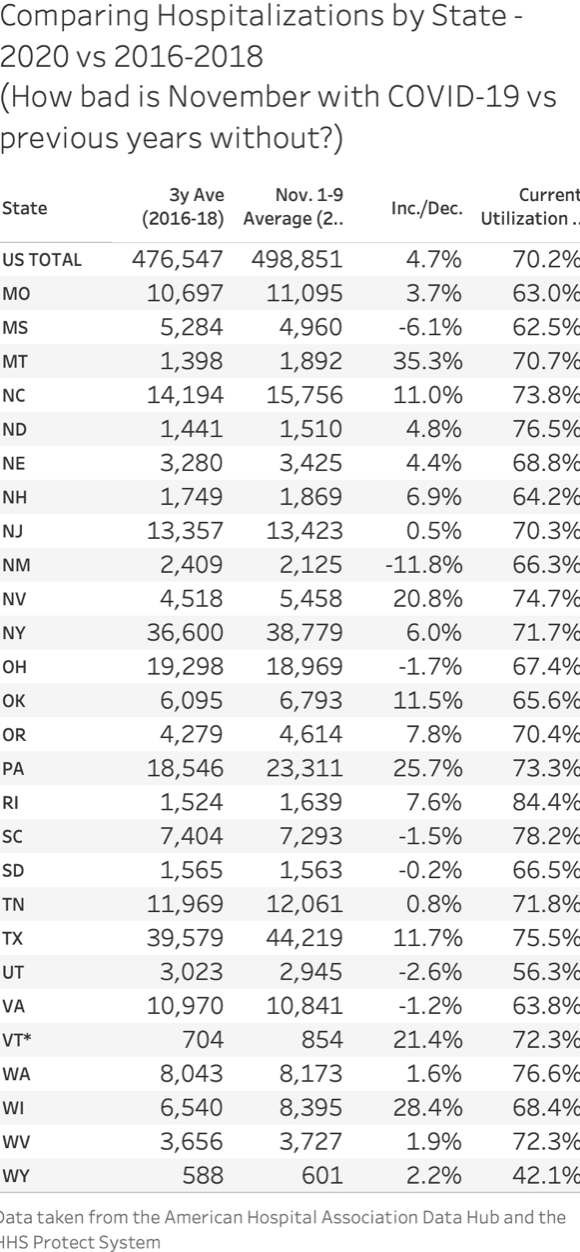
People are appropriately concerned about the capability of hospitals to care for everyone who may need care as a result of CV-19 or otherwise. As I have explained before, the US has embarked on a concerted campaign for the last two decades to reduce inpatient hospital utilization, which means reduction of capacity and running at a high level of capacity utilization. This minimizes per stay costs. But it means that we don’t have a lot of empty hospital beds typically sitting around. I have also explained that most hospital beds can be used for most patients, and ICU typically means more intensive monitoring and equipment use, but for most patients a typical ward, if properly staffed, could serve the same purpose. So the line between ICU and regular hospital bed isn’t that stark. The charts below show current hospital utilization overall versus the average for the past three years by state. In general it looks okay. Partly this is because we aren’t seeing flu hospitalizations in typical numbers and people and institutions may have deferred certain hospitalizations. I agree with those who say staffing may be a bigger issue. But my parting thought is that in regard to the areas currently seeing a fall surge, this was very predictable given the typical seasonal pattern of coronavirus, governments have had many, many months to prepare for the likelihood of a fall surge and if we aren’t prepared it is completely due to an ineffective and incompetent government response to a known likely occurrence–a large number of cases in the fall, some percent of which would require hospitalization.



about staffing…
Warning, anecdotal: One of those large physicians’ consortium in my part of the world drastically reduced on-site services during the first part of the panic. After bean counting, they then reduced non-physician staff by over 50% … and haven’t built it back up since. Maybe it’s the same elsewhere?
In his press conference announcing the Stay Home order last Spring, Governor Walz said there were fewer than 250 ICU beds in Minnesota when we were projected to need 3,000; therefore, we needed two weeks to flatten the curve to avoid overwhelming them. In his press conference announcing the first extension of the Stay Home order, Governor Walz applauded the hard work done by health care providers and government officials – we now had 3,000 ICU beds available on 72 hours notice; however, ventilators were still on back-order, so he needed to extend the lock-down to avoid overwhelming the few fully equipped ICU beds we had.
Last week, the Governor announced new restrictions – basically cancelling Thanksgiving – because rising numbers of hospitalizations may overwhelm the system. But the Star Trib reported last week: “COVID-19 ICU admissions have doubled since late September but still make up only 18% of ICU usage. Most of the 1,140 patients in Minnesota ICU beds are recovering from surgeries or being treated for unrelated issues such as strokes and traumatic injuries.”
1,140 patients in ICU beds is a third of the ICU beds Governor Walz claimed we could have. What happened to the other 2,000 ICU beds?
QUESTION: Has the criteria for hospital admittance and dismissal of patients with COVID changed since spring?
<" if we aren’t prepared it is completely due to an ineffective and incompetent government response to a known likely occurrence"
Kevin, two questions.
1. How can state and local governments create more healthcare personnel?
2. Are most of the hospitals in MN state owned or privately owned?
I don’t think it is a matter of creating new personnel, although they are graduating at a regular pace, it is deploying the very large workforce that exists, many of whom work part-time or as temps, to where you need them. The state says they have done that, if true, then reassure people instead of frightening them. Hospitals are largely non-profit in Minnesota, a few government owned ones,
I agree with Bob Easton in his post that with the reduction in hospital or clinic revenue staffs have been furloughed or permanently reduced due to lack of patients. This reduction falls into the demo of most Medicare patients who are in the highest Covid deaths category. Very interesting read and yes makes you wonder what is really reported in this the yellow journalism part II era.
According to North Carolina DHHS 11/16/20
25,466 hospital beds statewide: in use 14,900 (58.5%), staffed unused 5924 (23.3%), unstaffed or don’t know 4642 (18.2%), corona beds 1424 (5.6%)
3489 ICU beds statewide: in use 1785 (51.2%), staffed unused 604 (17.3%), unstaffed or don’t know 1100 (31.5%) corona ICU beds 360 (10.3%)
FYI: With approximately 40% (4,644,683) of NC’s population tested (March-Nov), 6.8% have tested positive for corona virus. This total % has remained constant for the last 6 months.
Reassure them of what? That the Star is going to provide all available resources to respond to the pandemic? Duh!
Kevin, here is the problem I see for the position you’ve taken on the pandemic. Since the beginning you have maintained that government officials have greatly exaggerated the risks of COVID-19. Now that cases are riding you are now espousing the position that if hospital resources are overwhelmed it is due to the incompetence of government.
Can you see why that is not an intellectually tenable position?
So it isn’t possible to both exaggerate the risk to the general public, which I have repeatedly tried to show is low using the state’s actual data, and have an incompetent epidemic response? Sorry, not seeing how that has any logical inconsistency. And it clearly is the case in Minnesota, when you consider the overall impact on people’s health, economic, social and educational well-being. See the article this morning about how many St. Paul high schoolers have just totally checked out? Is that a sign of a responsible epidemic response? The inconsistency would be if the state has been constantly stressing how dangerous and widespread the epidemic is and then isn’t prepared for a case surge that they now say they have been telling us for months was coming. To be fair, the state actually does say in the briefings that they have a plan and believe there will be adequate capacity, and I believe that is the case. So if they emphasize that and try to keep people calm and remind them that for 99% plus of the population this is at worst a mild disease, that would be a better overall message. You see the headlines.
What of the educational system….just how many kids across the board have ‘checked out’. My fantastical guess is that boatloads have, especially those who were at the margins already. That’s acceptable though, as it will reduce class sizes.
I am wondering if the increased hospitalizations are cases that in the spring would not have been admitted due to the faulty models and concern about hospital capacity. Are we really having more cases as compared to the spring, when this massive testing wasn’t occurring, and people were told to just stay home if they didn’t meet the testing criteria?
I think everyone who needed to be hospitalized got hospitalized in the spring. I am trying to do some analysis to “normalize” cases across the epidemic, to make a better comparison of hospital and death rates. Don’t know how accurate that can get, but it would help understand if there are fewer hospitalizations and deaths per case now. My raw cohort trend analysis, which I am also in the process of updating, would suggest that hospitalizations and deaths as a function of cases have generally declined over the course of the epidemic, which is generally what you would expect, as there is a learning curve on how to best treat any new disease, and there may have been front-loading. That said, I believe we may see increased hospitalizations solely due to remdesivir administration and we are seeing more “observational” stays, which tend to be very short.
Treating a Covid patient in the ICU is an incredibly labor-intense project. It might take four to six staff members, all gowned to the hilt, just to turn the patient over and wash them every day.
Patients who are put into a coma might require this level of care for many weeks. I had a collapsed lung two years ago and spent five days in an ICU. I lost track of how many staff members it took to care for me, and that was when no one needed to wear hazmat suits.
In other words, it does not take much to overwhelm the hospital system. It would not be shameful to say that some patients cannot be saved — although a medical professional would end their career with such honesty.