You may recall that eons ago, early on, I wrote a number of posts on the Minnesota model of the epidemic, its flaws, why it was, and was going to be, so far off, (all accurate criticisms by the way) and if you are going to critique someone’s work, you should see if you can come up with a better model, so I tried to. Here is that schematic, with a few thoughts on how what I have learned would change it. The new text is in a different color, I hope. This is actually a modification of a repost that I did about a month after the first version went up.
The reason I am reposting this is because the emerging research supports the idea that there is a sizable contingent of people who don’t get infected. Because of that we likely get to population immunity quicker and even fewer people are exposed. My current guesses, and that is all they are, is that about 30% to 40% of people won’t be exposed; about 25% or so won’t be “infected” if exposed; around 30% will be asymptomatic or mild illness and the remainder will have moderate to serious illness. When we understand the true prevalence, I think the rate of hospitalization will be 1% to 2% and the fatality rate will be maybe .1% to .2%. Again, just guesses. Hmmm, I have thought more about what it means to be “infected” and the actual physical nature of interaction with the virus (this is reflected in several posts over the past few weeks). Now I would say everyone could be exposed, but if we define “infected” as the virus entering into cells and replicating and creating significant additional virus particles that are exhaled, so that they are “infectious”, there is a large group of people who don’t get infected, largely because their immune systems, either due to innate capabilities or an adaptive response to prior coronavirus infections, repulse the virus very quickly upon contact, with most clearing it at the mucosal level. So I would now estimate that around 25% to 35% of people are likely to be infected and infectious after exposure. I stand by my hospitalization and fatality rate predictions, in fact they may be high. In terms of population immunity, while everyone could be exposed, once transmission slows significantly, due to a combination of the group that doesn’t get infected, plus the group that is infected and has an adaptive immune response, plus some behavioral changes, like isolating the most vulnerable populations, then the likelihood of exposure will also become much lower, so some people may never be exposed. I am going to post updated perspectives on population immunity separately, but I think transmission slows dramatically after around a 20% level of actual CV 2019 infection.
So here is my updated schematic to aid in thinking about the outcome of the coronavirus epidemic. The flow is basically the same as in the original chart but the look is a little different.
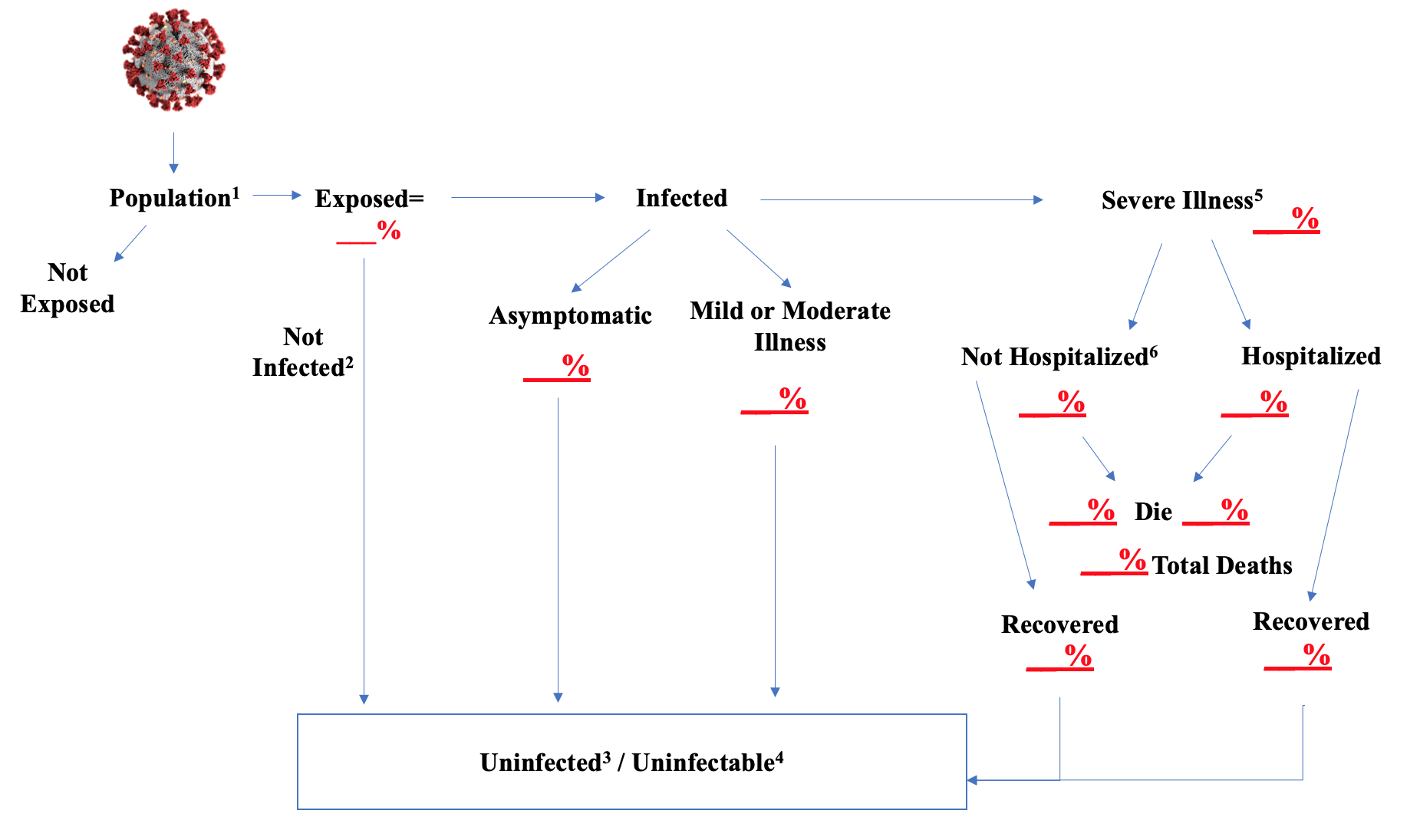
The footnotes give an explanation of issues related to certain steps.
- The population is whatever group you want to run the model against. It could be the country; or the state of Minnesota and many other states have models for their population. When you load the population into the model you should give it the relevant characteristics in the same proportion that they exist in the real world. So age, sex. Since this disease seems worse in dense areas, the population density of place of residence. People with underlying health conditions are more vulnerable, so those should be loaded in. Residential setting seems very important; a high percent of people in nursing homes and other senior living group settings are getting seriously ill and dying. The more characteristics that seem linked to disease and mortality risk you can load into the population in the model, the more accurate your results are likely to be. If one group seems particularly vulnerable, you might pull it out and model it separately. That should be done for senior group living settings for this virus epidemic. If you were doing agent based type modeling, you would assign everyone several numbers, perhaps on a one to ten scale. One for susceptibility to infection. One for demographic variables, like age, comorbidities, type of residence, etc. One for contact level. You would estimate what percent of the population gets what number and then you would build your transmission formulas around those.
- I think there is strong evidence that many people, even after being exposed to the virus, do not develop an infection. I would now caveat this as above, with a clearer definition of “infected”. Children in particular fall into this category. Several studies in situations of close, extensive contact with the virus, find that a number of people who must have been exposed are not being infected. There could be several explanations for this phenomenon. One is that the “dose” was too low. To cause an infection, a person may need to take into their body a certain number of virus particles. That dose likely varies extensively by person. A healthy young person may not be infected even after exposure to a massive dose. It probably only takes a very small dose for a fragile senior in a nursing home to develop the disease. Some people may have antibodies to other coronaviruses that are capable of aiding in warding off this strain. Recent research shows that this is almost certainly the case. Some may have genetic variations in the receptors that the virus uses to gain entrance into cells or other genetic variations that make them more or less susceptible. And there may be other protective mechanisms that we simply don’t understand. If you knew what these reasons were, you could just build them into the population characteristics, but they would still then just not ever be infected.
- This “Uninfected/Uninfectable” bucket is designed to be one of “destinations” for people who have run all the way through the model. Unfortunately, the other one is death. The Uninfected is the group that we just discussed. It is conceivable that at least some of this group, could yet be infected, if the issue is dose. Someone who was exposed but the dose just wasn’t high enough, could later become infected if they encounter a higher dose. I doubt this would happen very often, but it could occur. Yeah, unfortunately, adaptive immunity, or an initial fending off of the virus, should not be thought of as an absolute barrier.
- “Uninfectable” refers to persons who have been exposed and survived and so presumably have antibodies or immunity against re-infection. There may be Uninfected persons who are also Uninfectable, if, for example, there are people with cross-reactive antibodies or genetic variations that are protective. I recognize that there may be a question about the durability and strength of antibody development, particularly in those who are asymptomatic or have mild illness, although the most recent research, which I will post on separately, does not find this to be the case. Even clearer now that even people with mild infections develop robust immune responses, both B cell and T cell related, and that protection will likely be long-lasting and will allow them to quickly dispatch of the virus on any re-exposure.
- My gradations of severity of illness are “Asymptomatic”, these are people who became infected but are not showing any symptoms of the disease; Mild or Moderate Illness–these people had symptoms, may have sought some medical care, but whose condition would not warrant hospitalization; and Severe, which by definition is those whose condition did warrant hospitalization. The Asymptomatic and Mild or Moderate Illness groups all go to the Uninfected/Uninfectable bucket at the conclusion of their illness. These buckets have held up well.
- Although the Severe Illness group is defined as warranting hospitalization, there will be those who do not go to the hospital. Many people, especially older patients, may have advance directives which limit the care to be given to them, including hospitalization. Others may have surrogate decision-makers who don’t want the patient hospitalized. And some will have such rapid exacerbation of the disease that they do not make it to the hospital. We know people are dying at home; we don’t know how many or why. Very, very clear now that advance directives are playing a role in deaths.
The schematic can be viewed as an end-state, or as the basis for creating formulas to drive the population through the flow. A few observations. Some part of the population is not going to be exposed. This typically is related to the infectiousness or transmissibility of the virus or other infectious agent. The more infectious, the more people need to have some form of immunity before transmission effectively ceases. There are formulas to calculate this, but it might not be unlikely to believe that for this strain of coronavirus, immunity needs to rise to 80% or so of the population. But also remember that there appears to be some percentage of the population which simply doesn’t become infected even after exposure. So it is the total of those people with antibodies and those who don’t become infected that may stop transmission. See my additional remarks above regarding population immunity and transmission.
Determining the speed of the spread into the exposed bucket and then out into the infected and serious illness buckets is also a critical part of any formulas. There appears to be a fairly well understood incubation period of about 5 days to develop symptoms. It is less clear how long it takes to determine that someone will need hospitalization. Determining the spread from infected people to the unexposed population is typically done by contact models, but these often don’t take some critical factors into account, as I mentioned in the comments about the “population” above. This transmissibility factor is very important. The CDC is now publishing parameters, and their are other studies which give us time lags to hospitalization or death, for example.
The biggest unknowns in regard to this epidemic are what percent of the people fall into that uninfected after exposure bucket and what percent are asymptomatic or have mild to moderate illness. I am not sure how to establish the former, it is fairly clear it exists, but to what extent? The latter can be established by the kind of combination infection/antibody studies we are beginning to see results from. It is apparent from those results that a very, very small percentage of the total infections result in serious illness. Estimates are coalescing around maybe 10% of cases being detected. I think as testing has spread, that is too low. People use different definitions of asymptomatic and mild illness, but the combination of the two accounts for over 95% of all cases.
I am assuming unmitigated spread. If you are concerned about impact on health resource capacity, you would look at your daily runs of the model and compare the people who are hospitalized, need ventilators, need the ICU, etc. to your capacity. I have elsewhere given my views on the likelihood of this occurring. If you desire to, you can model the effects of mitigation tactics, primarily by modifying your formulas for how the infected mix with the unexposed population. Despite modeling based terrorization, no where did anyone suffer because we lacked adequate health resources.


This is the type of information that should be distilled and put into terms that the average person can understand. Unfortunately, that hose left the barn a long time ago. It was and is political so the goal was scare the hell out of everyone and even when new information becomes available attack anyone who advances knowledge; even have them kicked off the internet. I would also add that virtually no one in prime time is talking about strengthening the immune system and how to do it. I am 68 years old and have been intentionally building my immune protection for years. But, as you well know there is no money in prevention. Which leads me to another point, vaccine.
Vaccines will become available in short order because once again its about money and politics. Science only matters when it advances the lefts agenda, which is power, control and money. Your work IS important but unfortunately is not going to reach the general public and even if it could the impact would be almost null. Politicians and health officials have effectively scared the public into panic. They will do anything they are told.
Kudos to you, Kevin. The level of analysis put forward here surely evinces the amount of personal time, energy, and dedication you spend on this disease.
Impressive.